IMPORTANT CHANGES ARE COMING...
Effective October 1, 2020, most people will get the same Medicaid services in a new way – through new health plans. The Department of Health Care Finance (DHCF) intends to award three new contracts to the following health plans:
- AmeriHealth Caritas District of Columbia, Inc.,
- MedStar Family Choice, and
- CareFirst BlueCross BlueShield Community Health Plan District of Columbia (formerly known as Trusted Health Plan).
Medicaid benefits will stay the same, in fact beneficiaries may receive more services. There are no changes to eligibility. Coverage and care will not be interrupted.
Beneficiaries may be assigned to a health plan on October 1, 2020. Beneficiaries will receive more information telling them which health plan they are assigned to and how to change health plans, if they so choose. DHCF is currently in the process of finalizing contracts with the health plans. Please click here for more information and updates.
In early-August, DHCF sent a postcard to beneficiaries currently enrolled with a health plan informing them about the upcoming change.
Provider Information
- DC Medicaid Provider Resource Guide [PDF]
- MCO Provider Pharmacy Forum - November 19, 2020 [PDF]
- DC MCO Dental Provider Forum Presentation [PDF]
- MCO Provider Forum Presentation [PDF]
- MCO Provider Forum [PPTX]
- Provider Hotline Letter [PDF]
- Pharmacy Benefit Continuity of Care [PDF]
- Provider Continuity of Care Letter [PDF]
- Managed Care Provider FAQ [PDF]
- Behavioral Health Provider FAQ [PDF]
- FY21 MCO Provider Reimbursement Letter [PDF]
During the transition period – or from now until December 31, 2020, MCOs will reimburse for services rendered to covered beneficiaries regardless of your contracted status with the MCO.
Providers are encouraged to call 1-877-685-6391 with questions.
Medicaid Reform
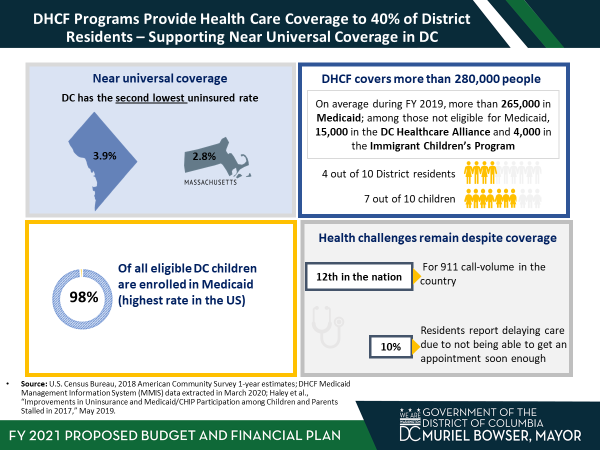
Over the past several years, the District of Columbia has made significant improvements in providing healthcare coverage to District residents. DC’s uninsured rate of 3.9% is second lowest in the country, behind Massachusetts. DC Medicaid, Health Care Alliance and Immigrant Children’s Program provide healthcare coverage to over 280,000 individuals, nearly 40% of District residents. However, health challenges remain despite high levels of healthcare coverage. Over the next five years, DHCF is undertaking an ambitious plan to transform the Medicaid delivery system to improve health outcomes.
Reform Focus
- Value over volume
- Better coordinated care
- Increased access to care
Reform Path
2020
- Implement New Behavioral Health Services: dhcf.dc.gov/1115-waiver-initiative
- New Managed Care Contracts
- Fee-For-Service Transition to Managed Care: dhcf.dc.gov/ffs-transition
2021
- Implement Program of All-Inclusive Care for the Elderly (PACE): dhcf.dc.gov/page/pace-dc
2022
- Increase coordination between Medicare and Medicaid via Highly Integrated Dual Special Needs Plans (HIDE-SNP)
2025
- New Managed Care Contracts that include Long Term Care Services and Supports (LTSS)
- Increase coordination between Medicare and Medicaid via Fully Integrated Dual Special Needs Plans (FIDE-SNP)
This page will be updated with more information as it becomes available, and you may subscribe to email updates by contacting [email protected].


