Innovation - Triple Aim
SIM States
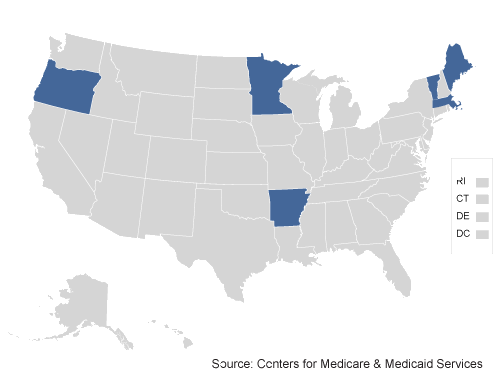
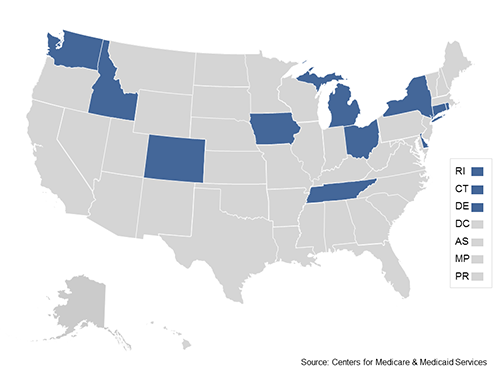
The State Innovation Models Initiative provided funding to support the development and testing of state-based models for multi-payer payment and health care delivery system transformation with the aim of improving health system performance for residents of participating states. Six states were awarded Model Test Awards in Round One and are actively testing their models. Eleven states were awarded Model Test Awards in Round Two.
Round One Test States
Arkansas
In the state of Arkansas, persons with complex or special needs (e.g., developmental disabilities) will also have access to health homes, which will work with their medical homes to coordinate medical, community, and social support services. Payments will include performance-based care coordination fees, as well shared savings for medical homes based on their ability to reduce total cost of care while also achieving goals for quality.
Arkansas will also continue to institute and expand its system of episode-based care delivery for acute, procedural, or ongoing specialty care conditions, using a retrospective payment approach that will reward providers who deliver high-quality, cost-effective and team-based care across an entire episode of care.
Maine
The state of Maine will test its plan for improving the quality of health care and improving the health of all citizens by aligning benefits from MaineCare (the state’s Medicaid program) with benefits from Medicare and commercial payers to achieve and sustain lower costs for the Medicaid, Medicare and CHIP populations while maintaining access to care, improving care quality, and improving patient satisfaction.
The Maine innovation model will support the formation of multi-payer Accountable Care Organizations (ACOs) that commit to providing greater value in return for performance-based payment for high quality care. These ACOs will agree to meet established quality standards for clinical care and publically report on their performance. Through the provisions of the plan, Maine will support and strengthen enhanced primary care; support and strengthen alignments between primary care and public health, behavioral health, and long-term care; support the development of new workforce models for the transformed system; and align measures, data and analytics across providers. In addition, the State of Maine will implement payment reform across public/private payers; spread the patient-centered medical home model of enhanced, integrated primary care; and achieve transparent understanding of the costs and quality outcomes of patients across all payers statewide.
Massachusetts
In the Massachusetts model, primary care practices will be supported as they transform themselves into patient-centered medical homes—capable of assuming accountability for cost and offering care coordination, care management, enhanced access to primary care, coordination with community and public health resources, and population health management. The Massachusetts model will strengthen primary care through shared savings/shared risk payments with quality incentives based on a statewide set of quality metrics, as well as payments to support practice transformation.
This award will be used to support public and private payers in transitioning to the specified model; to enhance data infrastructure for care coordination and accountability; to advance a statewide quality strategy; to integrate primary care with public health and other services; and to create measures and processes for evaluating and disseminating best practices.
Minnesota
To better integrate care and services for the whole person across the continuum of care (including health care, mental health care, long-term care and other services), the Minnesota Accountable Health Model will test a comprehensive, statewide program to close the current gaps in health information, create a quality improvement infrastructure, and provide the workforce capacity essential for team-based coordinated care. In addition to strengthening clinical health care, the Minnesota model for health system transformation will emphasize community health, preventive services, behavioral health, and other support services.
Minnesota ACOs will create linkages between Medicare, Medicaid, and commercial insurers, aligning payments to provide better care coordination, wider access to services, and improved coverage. Minnesota also plans to work with community organizations to create “Accountable Communities for Health” that will integrate medical care with behavioral health services, public health, long-term care, social services, and other forms of care, share accountability for population health, and provide care centered on the needs of individuals and families.
This award will enable Minnesota to expand its health information exchange and health information technology infrastructure, develop a workforce of community health workers and care coordinators, and support primary care physicians who wish to transform their practices into Patient-Centered Medical Homes to improve their patients’ overall health.
Oregon
The Oregon Coordinated Care Model (CCM) will focus on integrating and coordinating physical, behavioral, and oral health care; shifting to a payment system that rewards quality care outcomes rather than volume; aligning incentives across medical care and long-term care services and supports; reducing health disparities and partnering with community public health systems to improve health.
Oregon will begin implementing its model test in Medicaid through its system of Coordinated Care Organizations (CCOs)—risk-bearing, community-based entities governed by a partnership among providers of care, community members, and entities taking financial risk for the cost of health care – and use the State Innovation Models Initiative funding to foster the spread of this new model of care to additional populations and payers, including Medicare and private plans, such as those covering state employees. CCOs have the flexibility, within model parameters, to institute their own payment and delivery reforms to achieve the best possible outcomes for their membership. They are accountable for the health and care of the population they serve and are rewarded for improving both the quality of care and health care value. CCOs will transition payment for care from a fully-capitated model to payment that is increasingly based on health care outcomes. To accelerate the transition, the Oregon Health Authority plans to create a Transformation Center that will disseminate best practices among CCOs and other health plans, support rapid cycle improvement, and spread the model across payers and into the qualified health plans of the health insurance exchange in 2014.
Vermont
The state of Vermont will: increase both organizational coordination and financial alignment between clinical specialists and Vermont’s Blueprint for Health advanced primary care practices; implement and evaluate value-based payment methodologies; coordinate with other payment reforms on developing a financing and delivery model for enhanced care management and new service options for Vermonters eligible for Medicare and Medicaid; and accelerate development of a learning health system infrastructure that will support delivery system redesign and state evaluation activities.
Vermont will achieve these goals through three models: a shared-savings ACO model that involves integration of payment and services across an entire delivery system; a bundled payment model that involve integration of payment and services across multiple independent providers; and a pay-for-performance model aimed at improving the quality, performance, and efficiency of individual providers.
Round Two Test States
Colorado
Colorado’s plan, entitled “The Colorado Framework,” creates a system of clinic-based and public health supports to spur innovation. The state will improve the health of Coloradans by: (1) providing access to integrated primary care and behavioral health services in coordinated community systems; (2) applying value-based payment structures; (3) expanding information technology efforts, including telehealth; and (4) finalizing a statewide plan to improve population health. Colorado will integrate physical and behavioral health care in more than 400 primary care practices and community mental health centers comprised of approximately 1,600 primary care providers. In addition, the state will work to establish a partnership between their public health, behavioral health and primary care sectors.
Connecticut
Connecticut’s plan utilizes several statewide and targeted interventions to: (1) improve population health; (2) strengthen primary care; (3) promote value-based payment and insurance design; and (4) obtain multi-payer alignment on quality, healthy equity, and care experience measures. Specifically, the state will implement a Medicaid Quality Improvement Shared Savings Program (MQISSP). Primary care providers participating in the MQISSP will benefit from programs designed to enhance primary care capacity in the state, including learning collaboratives to foster continuous learning. Connecticut will implement Health Enhancement Communities and Prevention Service Centers focused on improving population health. The state will develop a core quality measurement set for primary care providers and select specialists that will capture a cross-payer measure of care experience tied to value-based payment in a common provider scorecard.
Delaware
Delaware will: (1) support ten community-based population health programs (Health Communities); (2) develop an IT infrastructure to support a cross-payer scorecard of core measures available to providers with related tools for patient engagement and price and quality transparency; and (3) engage payers in the development of a pay-for-value model and a total-cost-of-care model for providers (including independent PCPs), with the goal of attributing all Delawareans to a primary care provider during the performance period. Delaware will implement workforce development strategies to build competencies and address the current workforce and will also develop educational programs to address the needs of model participants.
Idaho
The state of Idaho will achieve state-wide health care system transformation that will deliver integrated, efficient and effective primary care services through patient-centered medical homes (PCMH). Specifically, Idaho will build 180 Nationally Recognized PCMH practices, including 75 Virtual PCMHs, by the end of the Model Test. Practices will be selected from each of the seven Health Districts in Idaho during the test period. The state will also support providers through expanded connectivity via electronic health exchange, and by aligning the support of public and private payers to accelerate practice transformation.
Iowa
Iowa’s plan for health system transformation builds upon the ACO model that currently covers the state’s expanded Medicaid population, called the Iowa Health and Wellness Plan. This population-based model also will align with quality measures and payment methodology (shared savings and calculation of total cost of care) utilized by the Wellmark commercial ACOs. By the end of the performance period, the Medicaid ACOs will be accountable for the long term care and behavioral health services of their attributed patients. The state also will leverage and spread existing community transformation initiatives focused on the social determinants of health.
Michigan
The state of Michigan will implement its Blueprint for Health Innovation with the creation of Accountable Systems of Care (ASC). ASCs will be networks of providers utilizing patient-centered medical homes supported by payment models that align incentives. The ASCs are further supported by Community Health Innovation Regions (CHIRs), which are cross-sector partnerships that address population health and connect patients with relevant community services.
New York
The state of New York will adopt a tiered Advanced Primary Care (APC) model for primary care. This model will include behavioral and population health, and be complemented by a strong workforce and engaged consumers, with supportive payment and common metrics. The state will: 1) institute a state-wide program of regionally-based primary care practice transformation to help practices across New York adopt and use the APC model; 2) expand the use of value-based payments so that 80% of New Yorkers are receiving value-based care by 2020; 3) support performance improvement and capacity expansion in primary care by expanding New York’s primary care workforce through innovations in professional education and training; 4) integrate APC with population health through Public Health Consultants funded to work with regional Population Health Improvement Program contractors; 5) develop a common scorecard, shared quality metrics and enhanced analytics to assure that delivery system and payment models support three-part aim objectives; and 6) provide state-funded health information technology, including greatly enhanced capacities to exchange clinical data and an all-payer database.
Ohio
The state of Ohio will transform the state’s health care system by rapidly scaling the use of patient-centered medical homes (PCMHs) and episode-based models and by developing cross-cutting infrastructure to support implementation and sustain operations. By the end of the Model Test, Ohio plans to launch 50 episodes of care and implement PCMHs statewide. In addition, the state is focused on incorporating population health measures into regulatory and payment systems in order to use those measures to align population health priorities across clinical services, public health programs, and community-based initiatives.
Rhode Island
The state of Rhode Island will implement a population health plan based on the results of community health assessments, including the integration of primary care and behavioral health. In addition, the state will expand the use of health homes by providers in the state, thus serving a substantial majority of the state’s population. In order to facilitate and support much of this transformation activity, the state will establish a Transformation Network to provide technical assistance and analytical capabilities to payers and providers participating in the value-based models. The state will augment its HIT infrastructure to include an all-payer claims database, statewide health care quality measurement, patient engagement tools, and state data management and analytics.
Tennessee
The state of Tennessee will execute multi-payer payment and delivery reform strategies. The state will accelerate transformation in primary care by developing pediatric and adult PCMHs and health homes that will integrate value-based behavioral and primary care services for people with Severe and Persistent Mental Illness. In addition, Tennessee plans to implement 75 episodes of care over the test period. Tennessee will also implement quality and acuity-based payment and delivery system reform for long-term services and support (LTSS), targeting nursing facility services and home and community based services for seniors and adults with physical, intellectual and developmental disabilities. Finally, the state is planning to develop a statewide plan for improving population health in order to address disparities and state-specific population health needs.
Washington
The Healthier Washington project will move health care purchasing from volume to value, improve health of state residents, and deliver coordinated whole-person care. The State will make targeted investments in the following areas: (1) community empowerment and accountability, through the implementation of regionally organized Accountable Communities of Health; (2) practice transformation and support through a “support hub”; (3) payment redesign, through shared savings and total cost of care models in collaboration with delivery system and payer partners; (4) analytics, interoperability and measurement; and (5) project management, through a public-private leadership council with a dedicated interagency team and legislative oversight.
Other Resources on SIM States
- State Innovation Models Initiative: Model Design and Pre-Test Round One final evaluation report [PDF]
- State Innovation Models Initiative: Model Test Awards Round One First Annual Report [PDF]
- Conducting the Orchestra of Multi-Payer Payment Reform: Achieving Harmony in Arkansas and Vermont (Blog)
- State Innovation Models: Early Experiences and Challenges of an Initiative to Advance Broad Health System Reform [PDF]
- CMS—Engaging Multiple Payers in Payment Reform (JAMA)
- Beyond a Traditional Payer — CMS's Role in Improving Population Health (NEJM)


